Treatment of burn injuries
This chapter will focus on treating mild-moderate burn injuries as these are most commonly encountered. We will not detail the most severe burn injuries requiring intensive care and extensive surgical reconstruction. We will not discuss burn injuries to airways or intoxication from inhaled poisonous smoke.
You will find the international recommendations for treating burns here. We also overview other treatment options that may be applied when not all resources are available.
The most important general principles in the treatment of burns are:
Cool down the injured skin as soon as possible using running, temperate water. In adults, we use the 20/20 rule ( 20 degrees Celcius water for 20 minutes). In children, we apply the 28/20 rule ( 28 degrees Celsius water temperature for 20 minutes) to avoid hypothermia. Remember that cooling down the injury has a positive effect within three hours from the point of injury. This means that if the patient arrives at your clinic two hours after the sustained burn and has not had the chance to cool the skin, you should do so on arrival at the clinic.
Pain treatment: assess the pain level and determine whether oral ( or rectal) pain medication may be sufficient. There may be a need for intravenous ( intramuscular) analgetics. If the patient is in severe pain, you will have to provide opioid-type analgetics, for example, morphine 0,05-0,1mg/kg. You should start with a low dose and slowly titrate upwards after about 5-10 minutes. Always have an antidote for opioids close by when delivering opioids to burn patients.
Severity assessment of the burn injury: Determine the percentage area of the burnt skin and the depth of the burns ( partial- or full-thickness burn injuries). Do not stress too much trying to differentiate between superficial partial-thickness and deep partial-thickness injuries. This is not so important at this stage and can be difficult to distinguish at the start. Burns affecting 10 percent of a child's body and those affecting 15 to 20 percent of an adult's body are considered major injuries and require hospitalization and extensive rehabilitation where these resources are available.
We advise the opening of all blisters. About a decade ago, there was a lot of discussion about this on an international level. Those who were against opening blisters argued that by opening them, we are turning a sterile situation into a non-sterile situation. Today, most burn centers have agreed that opening burn blisters is recommended. Most blisters will open spontaneously anyway. More importantly, it seems that we can stop the blistering process by opening burn blisters. We have routinely opened blisters over the last 15 years and have very good experiences doing so. This also allows us to assess the severity of the burn better.
Remember that burn patients should receive a tetanus vaccination if the last vaccinations were longer than five years ago. If the vaccination status is unknown, you have to consider giving tetanus- immunoglobulin (TIG), and the patient has to go through the complete vaccination process. Do not use antibiotics as prophylaxis against tetanus. At the end of this chapter, we have provided you with a summary of the center's recommendations for disease control (CDC) for tetanus vaccination.
Remove jewelry, watches, and traditional ornaments, even if they are in an anatomical location far away from the burn. Many patients develop general edema in burns above 15% surface area. If possible, elevate the burnt area to minimize local edema.
Clean the burn area. In some cases, it may be enough to rinse over the burnt skin. At other times you may have to remove loosened skin rests. In dirty burn wounds ar where there are charred rests, you may have to scrub the wound clean. This may require additional analgesics. Preferably such procedures should be done under some form of sedation where this is available. In the following subchapter, we will discuss some of the dressing options you can use.
Treating first degree (superficial) burns
The treatment of superficial wounds is relatively easy. The most important aspects are the initial cooling of the burn under running water and pain treatment. It is usually not necessary to seek medical help when treating first-degree burns.
If the patient has much pain after cooling down with water, you can apply a local anesthetic lotion or salve - for example, 3% lidocaine lotion or 5% lidocaine salve. Note that these substances are absorbed to some degree through the skin, significantly damaged skin. Therefore, it is essential to know the dosage limits, especially in small children. Remember that local anesthetics are toxic at high doses. This is especially important when using more potent topical anesthetics like Emla cream, which contains lidocaine and prilocaine and is more readily absorbed through the skin. As a rule of thumb, one tube ( 5g) is the maximum dosage for a one-year-old child/day. Emla cream is contraindicated in children below three months.
If available, special burn gels with a cooling effect can be applied after cooling with water. Be aware that there exist a confusing variety of burn gels with very different ingredients. Some contain plant extracts like tea tree oil or aloe vera. Some patients may develop an allergic reaction ( contact dermatitis) from such ingredients. We are not saying that you should not use these products- we want you to be aware of the possibility that a few patients may react adversely to burn gels that contain plant products. It is advisable to keep these gels refrigerated for extra cooling effect when applied.
1% hydrocortisone creams are beneficial to treat first-degree burns. This can be quite painful, especially when larger areas are involved ( like sunburns on the back), and hydrocortisone will resolve the inflammation faster than other burn gels. 1% hydrocortisone is a mild steroid sold without prescription in most countries. If stored refrigerated, the hydrocortisone will also provide an analgesic cooling effect when applied. Usually, it is sufficient to apply the cream twice daily in a thin layer for about three days. A dressing is generally unnecessary but may prevent chafing between the skin and clothing.

Figure 1 There is a confusing variety of gels available for treating superficial burns. Some might work better than others. To date, we do not have an oversight of which products are available in Africa and which ones work best. They can be stored refrigerated to give a cooling effect when applied

Figure 2 In accordance with many current guidelines for treating burns, we advocate the opening of blisters. Not only will this give you better control of the severity of the burn, but opening blisters early will prevent them from getting as big as in the image above. In our experience, opening blisters leads to faster healing times. image copyright: pediatricfoam
Treating second-degree ( partial-thickness) burns
Ideally, one should consult a burn center in cases with partial-thickness burns in the face, hands, feet, and groin areas. The same applies to partial-thickness burns over larger joints like the knees or elbows. Burns affecting 10 percent of a child's body and those affecting 15 to 20 percent of an adult's body are considered major injuries and require hospitalization. We always consult with a burn center in these cases. For example, at the clinic where we work, we take pictures with our mobile phones and send these to the burn center for a quick evaluation. We are aware that such a service is not available in many areas in Africa. At most rural clinics on the continent, health care workers have to deal with quite serious burns themselves, and only the most severe burns get transferred to a higher level of service. In the chapter on " Useful links for burn care," we have provided you with a link with contact information to burn centers in various African countries.
As with all types of burns, we first have to cool down the burn area with temperated running water for twenty minutes if this has not been done beforehand. Remember that cooling down the burn area is considered effective within the first three hours from the point of injury. It is, of course, essential to cool down the affected skin as soon as possible, but sometimes this is not possible. If the patient arrives at your clinic two hours after the burn happened and it has not been cooled down, you should use twenty minutes to do so then.
Give the patient some form of analgesia before you start to inspect the burn. If the patient has moderate pain, paracetamol and codeine may be sufficient. You can also apply topical anesthetics onto the burn area - remember that these can be absorbed through the wound, and you have to respect age-related dosages for these substances. If the patient has more pain, consider giving opioids like morphine. In children or very distressed adults, you may need some form of sedation. Midazolam and Ketalar are suitable for this. Ideally, such substances should be administered by experienced healthcare workers, preferably by an anesthesia team.
Inspect the burn area checking for areas of deeper injury. This is sometimes hard to see during the initial assessment and will usually become more apparent in following evaluations. We aim to clean the wound, remove loose skin, de-roof blisters, and cover the burn with a non-adherent dressing at the first wound treatment.
When it comes to dressings, it is generally recognized that we should use slightly moistened gauze during the initial exudative phase- using a non-adherent contact layer between the gauze and the wound. In the second phase- the healing phase- a hydrofiber dressing containing silver is recommended. This should be left in place for as long as possible ( 2-3 weeks).
Dressing choice day 0-3 (5) - the exudative phase
When it comes to dressing choices for partial-thickness burns, we use two different dressing regimes according to the time frame. During the first 3-5 days, most partial-thickness burns will have quite a lot of exudate coming from them. In this phase, we use a non-adherent netting (contact layer) directly on the burn and cover this with several layers of gauze, which are slightly moistened. Commonly, either a vaseline impregnated mesh ( for example, Jelonet) or a silicone type netting ( for instance, Mepithel) are used. The gauze we place over this is moistened with saline and then wrung out so that it is only slightly moist. It should not be wet! We often place at least 3-4 layers of gauze over the burn area to accommodate for enough absorption of exudate - otherwise, we end up having to change the dressing more often. The layers of gauze are secured to the body using rolls of cotton gauze bandages or whatever you have available. It can be notoriously tricky to dress burn areas in the groin area or under the armpits; for example, bandages in these areas often become dislodged in the course of a day or two.
Usually, we do not need to change this dressing before the second or third day. Sometimes there is more exudate coming from the burn than we expected, and our dressings may need to be already changed the next day.
What about the use of silver-sulfadiazine (SSD)? You are probably aware that there is some international discussion on what role SSD has in burn care. Until about a decade ago, it was very commonplace to use SSD as the initial treatment for most burns. Most of us thought it was sensible to provide a soothing effect and, more importantly, protect the burn area from infection. It has in vitro activity against a wide range of burn wound microbial pathogens, including S. aureus, E. coli, Klebsiella species, P. aeruginosa, Proteus species, other Enterobacteriaceae, and Candida albicans. Note, however, that there have been reports of resistance of Pseudomonas aeroginosa to SSD, and not all strains of Klebsiella are susceptible either. Note also that although rare, there are some toxicity issues with SSD. Allergic reactions are reported to occur in about 5%. More serious side effects can occur when applied to large burn areas. Due to the sulfa moiety, hemolysis in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency and methemoglobinemia have been reported.
In many western countries, SSD is no longer used as the primary treatment for burns. Several studies have shown that it does not provide significant advantages over other treatment modalities. Most burn care centers prefer that we have not covered the wounds in SSD before referral as this can make assessing the severity of the burns more difficult sometimes. In addition, we are concerned about possible resistance development ( especially Pseudomonas aeroginosa) and, in rare cases, toxicological side effects.
SSD comes under many brand names and is readily available in most African countries. It is reasonably cheap and is still one of the most common methods of treating burns in Africa. It will take many years before other modalities in Africa will gradually substitute this method. It took about 10-15 years before this was gradually phased out in many western countries. If you are routinely working with burn care patients in Africa today, we challenge you to try using primarily vaseline gauze (petroleum jelly) on the burns instead of SSD. If you apply a thick enough layer of vaseline to the burn area, the gauze will hardly adhere to the damaged area making dressing changes relatively painless.
Our personal opinion is that SSD should not be routinely used as a primary treatment for burns in Africa. We believe, however, that it still has a place in burn care. We suggest that it be available as an alternative for the later stages of healing if we see possible infection problems.

Figure 3 During the initial exudative phase of partial-thickness wounds, we only need quite simple tools as dressings. To avoid the dressing adhering to the wound, a contact layer like vaseline impregnated mesh or a silicone-based mesh should be used in direct contact with the wound bed. This we cover with multiple layers of slightly moistened gauze. Use sterile saline or cooked water for this. Do not use regular tap water as this increases the chance of pseudomonas infection. Keep your dressing in place with a crepe cotton roll or a cotton wool roll.

Figure 4 Silver impregnated hydrofiber dressings like Aquacel Ag Burn ( left), and Aquacel Ag (right) are seen as a gold standard in treating partial-thickness burns today. Aquacel Ag Burn has the advantage that it is made of stronger material and can be left in place for up to three weeks. Although the manufacturer (Convatec) advises using regular Aquacel Ag for up to two weeks, we have routinely left it in place longer if it still adhered to the wound bed.
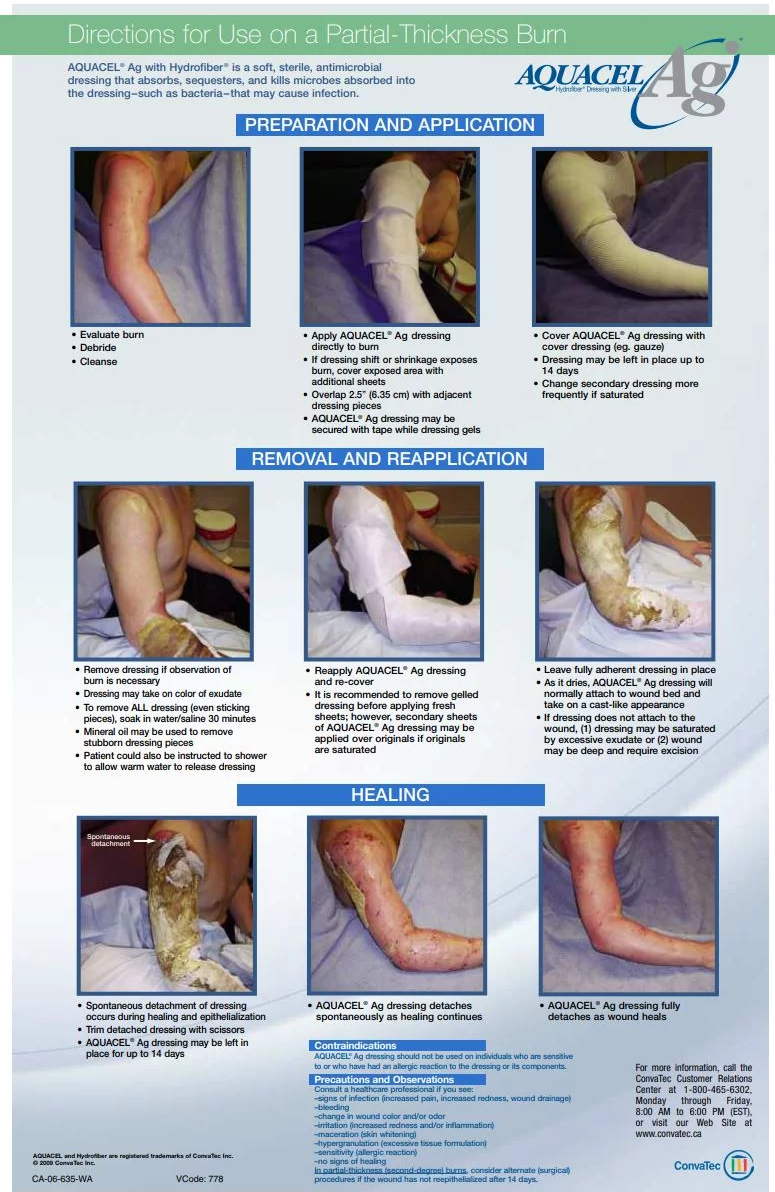
Figure 5 A guide to using Aquacel Ag dressings. The dressing is usually left in place for two weeks or more. As Aquacel dries, the dressing will adhere to the wound bed and takes on a cast-like appearance. The idea of leaving the dressing in place for as long as possible is not to disturb the epithelialization process. Equally important- we want to avoid painful dressing changes. Note - as you see in the picture on the bottom left, the appearance of the dressing looks somewhat "unappealing." If you have never used Aquacel before, this takes some getting used to. If the wound needs to be inspected earlier, the dressing should be soaked in water (saline) for at least twenty minutes before attempting to remove it. image copyright: Convatec
What alternatives can you use if you do not have access to a silver-coated hydrofibre dressing?
Since silver-coated hydrofibre dressings can be left in place for several weeks - they are not so expensive. Let's consider the expenditures used for changing dressings in a burn patient every third day ( including the costs of health care resources). A silver hydrofibre dressing is actually a cheap alternative! At least as important is the fact that it saves the patient from many painful dressing changes. So- if you can obtain these types of dressings, that is really what you should do.
We are aware that it is not realistic to expect silver hydrofibre dressings to be available in many parts of Africa in the near future. So what alternatives can you use? Ideally, the option you use should be something that does not adhere to the wounded and makes dressing changes excruciatingly painful. Polyurethane (PU) foam dressings with an inner silicone layer do not adhere as much and can be used, but these need to be changed more frequently depending on the amount of exudate. Although they do not adhere as much, dressing changes will still be somewhat painful even when using these. Also, the healing time will usually not be as fast as when using silver hydrofibre dressings. Furthermore, if your patient can afford silicone-coated PU foam dressings, they probably can afford a silver hydrofibre dressing.
What can you do if you have minimal resources and the only dressing type you have is cotton gauze? What you definitely should not do with cotton gauze is to place it directly onto the wound bed of the burn site. Without a doubt, it will adhere to the wounded, causing the patient unbearable pain during the removal. We are not supporters of the wet to dry dressing method here - it is simply not justified because it is a painful and outdated method of burn treatment. In addition, the healing of the wound is greatly disturbed every time we do a dressing change. If you only have gauze as a dressing, you will have to cover the burn site with some sort of barrier, which decreases the chance of adherence of the gauze on the wound bed. You can use simple vaseline for this. If you apply it in generous layers of about 5-10 mm thickness, the gauze will often not adhere to the wound bed. Burns react well to being covered with vaseline, and it also seems to decrease pain as the exposed nerve endings in the wound are covered with something smooth. Note that it is a good idea to cover the inner layer of the gauze with vaseline. This ensures that every inch of the gauze has a protective layer of vaseline on it. Furthermore, it is less painful to apply it this way rather than applying the vaseline directly to the burn site.
We would use vaseline in the early phases while there is still some exudate. Later on, as the burns become drier, you could switch to honey. Again, cover the burn site with a generous amount of honey before applying the gauze. It is absolutely possible to use honey in the early phases as well. However, because of the osmotic effect of honey, things can become a little messy if there still is a fair amount of exudate.
As we mentioned earlier, SSD has lost its position in burn care for various reasons. Many caregivers in Africa still use SSD on the burn and a gauze cover as the primary treatment. The SSD cream will rapidly absorb into the gauze, and the gauze will usually adhere to the wound bed in a couple of days. This method is painful for the patient, even if you apply the SSD cream in generous layers.
Gauze soaked in povidone-iodine is another method commonly used in many parts of Africa. While iodine undoubtedly protects against secondary infection, this method is basically a wet-to-dry dressing. As we mentioned earlier, this type of dressing is unnecessarily painful during change. Also, there is usually no need for a powerful antimicrobial agent such as povidone-iodine in these wounds unless they are infected.
There are many other improvised solutions out there - none of these have any documentation but are not considered harmful either. Mixtures of 50:50 vaseline and honey, vaseline and zinc paste, vaseline and povidone-iodine are examples of concoctions that some caregivers have successfully used in burn patients in Africa.
We are aware of studies showing the effectiveness of sterilized banana leaves and the flesh of papaya ( paw-paw) fruit to treat burns in Africa. We have not seen any of these methods in practice and will provide you with a link to articles describing these methods.

Figure 6 If you are interested in the use of sterilized banana leaves in burn care, you can click on the image of the article above Wafaa Gamel Ali, Hiat Abo Eazaym: The effectiveness of Using Banana Leaf Dressing in management of partial Thickness Burns Wound You will find several articles on the same subject by searching for " banana-leaves wound care" in a google search. image copyright: researchgate
Video 1 A video explaining the use of sterilized banana leaves in treating partial-thickness burns. Copyright Interburns.
Treating third-degree (full-thickness) burns
Third-degree burns should ideally be treated at a center experienced in burn care. Almost always, there will be a need for debridement and skin grafting. Again, in many parts of Africa, small areas with third-degree burns have to be handled at rural clinics. If there is someone with knowledge of debridement and small skin grafts, this is usually manageable. We will not go into more detail here on the treatment of third-degree burns as this will exceed the scope of this website. We have written a separate chapter on debridement and skin grafting - please also refer to these.
There can often be small patches of third-degree burns within an area that is otherwise a second-degree burn. If these patches are small- about 1 cm2 they can be observed. Sometimes they will form a dry scab which gradually heals away. At other times these areas start to open up as deeper wounds and need to be treated accordingly.

Figure 7 Larger areas with third-degree burns almost always need debridement and split-skin grafting. You should refer these patients to a center with surgical resources and experience in burn care whenever possible. image credit: africaburnrelief
Figure 8 Ideally, severe burn injuries should be treated at the highest level possible. The International Society for Burn Injuries has provided an interactive map showing the countries in Africa ( and globally) where specialized burn units are available. The contact information for these burn units is also provided. Click on the image above to get to their website. source: worldburn.org
The issue of Pseudomonas aeroginosa and burn wounds
Burn wounds have a lot of exudate initially. Pseudomonas aeroginosa is a bacteria that thrives excellently under moist and warm conditions. Therefore, it is not surprising that Pseudomonas can quite frequently cause trouble in burn wounds. The toxins the bacteria secrete are powerful proteinases that cause a vicious cycle of further skin breakdown and increased patient pain. Once Pseudomonas has established itself thoroughly on the wound bed, it can be challenging to eradicate. For this reason, it is sensible to use antibacterial dressings like silver-impregnated dressing to keep the bacterial concentrations at a low level- as a prophylactic. Honey is also a suitable antibacterial agent to prevent secondary infections. SSD is still popular in many parts of Africa. As mentioned earlier, we recommend other alternatives as SSD has several disadvantages. However, once Pseudomonas has established in the wound, a course of SSD- applied daily over about ten days will usually eradicate the bacteria. So yes, SSD still has a place in burn care- we just do not think it should be used routinely on every burn patient.
In cases with severe Pseudomonas infection with a lot of slime production, our choices become more limited. Silver-coated dressings usually do not work very well in such situations as the silver usually will not penetrate deep enough through the slimy exudate that is constantly renewed. SSD does not work well in these extreme cases either, as it is just "washed away" with the slimy exudate. Gauze soaked in 3,5 % vinegar and left for 20 minutes applied twice daily for ten days can work well here - but the vinegar can obviously cause pain upon application. Paradoxically we have seen that some burn patients have little pain when vinegar is used- so it is possible to test it on a small area first. It is also possible to use lower concentrations of vinegar - studies have shown that vinegar has antibacterial activity against Pseudomonas in concentrations as low as 1%. You can also drip lidocaine on the wound bed first and wait for about 5 minutes before applying the vinegar dressings. Make sure that you have dripped some lidocaine on the entire wound bed.
If the patient does not tolerate vinegar dressings, you may have to consider using povidone-iodine gauze dressings. Pivodine- iodine is effective against Pseudomonas, and we use it at 5% strength. To avoid it acting like a wet-dry dressing, the iodine-soaked gauze should be changed often to avoid painful dressing changes.
As a general rule of thumb - forget about long dressing intervals if you are dealing with a pseudomonas problem. If you have issues with Pseudomonas in the wound ( and this applies to all wounds heavily colonized with this bacterial strain), you have to do dressing changes at minimum daily, preferably even twice daily!
We have also written a separate chapter on Pseudomonas aeroginosa- please refer to that for more information.
Guidelines for tetanus vaccinations/booster dose
-
Evaluate the immunization status of the patient. Unvaccinated persons should start and complete a primary series with an age-appropriate tetanus toxoid-containing vaccine (i.e., DTaP, TdaP, Td) as currently recommended by CDC. Consider persons with an unknown or uncertain history of receiving prior doses of tetanus toxoid-containing vaccines to have had no previous tetanus toxoid-containing vaccine. They should complete a primary series. This is because early doses of toxoid may not induce adequate immunity but only prime the immune system. Persons who have completed a 3-dose primary tetanus vaccination series:
-
If the last dose of a tetanus toxoid-containing vaccine was received less than 5 years earlier, consider them protected against tetanus. They do not require another dose of tetanus toxoid-containing vaccine as part of the current wound management.
-
If the last dose of a tetanus toxoid-containing vaccine was received 5 or more years earlier, administer a booster dose of an age-appropriate tetanus toxoid-containing vaccine.
-
-
Assess the need for administering TIG for prophylaxis.
TIG provides temporary immunity by directly providing antitoxin. TIG can help remove unbound tetanus toxin but cannot neutralize toxins already bound to nerve endings. Persons who have contaminated and dirty wounds and are either unvaccinated or have not received a primary series of tetanus toxoid-containing vaccines should receive TIG for prophylaxis. The dose of TIG for prophylaxis is 250 IU administered intramuscularly. Persons with HIV infection or severe immunodeficiency who have contaminated wounds (including minor wounds) should also receive TIG, regardless of their history of tetanus immunizations. -
Do not use antibiotics for prophylaxis against tetanus.
Medical experts do not recommend antibiotic prophylaxis against tetanus. However, clinicians should observe wounds for signs of infection and promptly treat them if they detect signs of infection.

Table 1 Recommendations provided by the CDC for usage of Tetanus- Immunoglobin (TIG) in wound management. copyright: https://www.cdc.gov/tetanus/clinicians.html
Abbreviations: DTaP = Diphtheria and Tetanus toxoids and acellular pertussis vaccine; Tdap = tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis; Td = tetanus and diphtheria toxoids; TIG = Tetanus immune globulin
*Such as, but not limited to, wounds contaminated with dirt, feces, soil, and saliva; puncture wounds; avulsions; and wounds resulting from missiles, crushing, burns, and frostbite.
† DTaP is recommended for children <7 years of age. Tdap is preferred to Td for persons aged 11 years or older who have not previously received Tdap. Persons aged 7 years or older who are not fully immunized against pertussis, tetanus, or diphtheria should receive one dose of Tdap (preferably the first) for wound management and as part of the catch-up series; if additional tetanus toxoid-containing doses are required, either Td or Tdap vaccine can be used.
‡ People with HIV infection or severe immunodeficiency who have contaminated wounds (including minor wounds) should also receive TIG, regardless of their history of tetanus immunizations.
§ Yes, if ≥10 years since the last tetanus toxoid-containing vaccine dose.
¶ Yes, if ≥5 years since the last tetanus toxoid-containing vaccine dose.

























